Glecirasib Shows Promising Efficacy in KRAS G12C+ Advanced NSCLC
Those who have been previously treated for KRAS G12C–mutated advanced NSCLC may benefit from treatment with glecirasib.
“Glecirasib is a covalent, highly selective, and orally bioavailable KRAS G12C inhibitor. Promising efficacy has been observed in patients with multiple KRAS G12C mutated tumors, including NSCLC, colorectal cancer, pancreatic adenocarcinoma, and other solid tumors,” according to Yuankai Shi, MD, PhD.
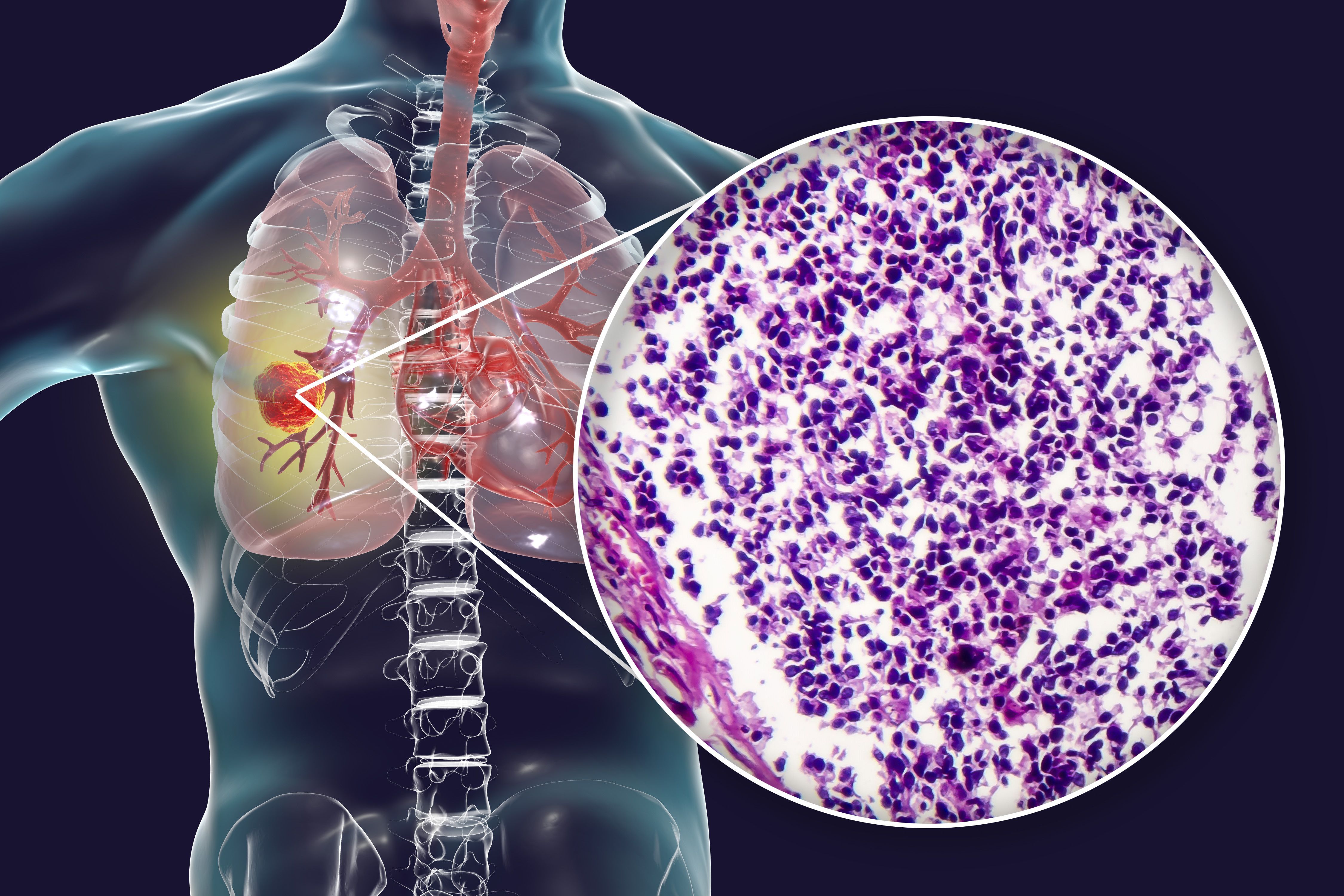
Promising efficacy was observed when glecirasib (JAB-21822) monotherapy was used to treat patients with previously treated KRAS G12C–mutant advanced non–small cell lung cancer (NSCLC), according to findings from a phase 2b trial (NCT05009329) highlighted in a presentation from the American Society of Clinical Oncology Plenary Series.
The confirmed objective response rate (ORR) with glecirasib was 47.9% (95% CI, 38.5%-57.3%), the complete response rate was 3.4%, the partial response (PR) rate was 44.4%, the stable disease rate was 38.5%, and the progressive disease rate was 10.3%. Data indicated that 3.4% of patients were not evaluable. Additionally, the disease control rate (DCR) was 86.3% (95% CI, 78.7%-92.0%).
“Glecirasib is a covalent, highly selective, and orally bioavailable KRAS G12C inhibitor. Promising efficacy has been observed in patients with multiple KRAS G12C mutated tumors, including NSCLC, colorectal cancer, pancreatic adenocarcinoma, and other solid tumors,” Yuankai Shi, MD, PhD, of the National Cancer Center/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College in Beijing, China, said in the presentation.
A total of 119 patients were enrolled to the single-arm phase 2b trial and received 800 mg of glecirasib once a day. The primary end point was ORR by independent review committee assessment. Secondary end points included ORR per investigator assessment, duration of response, DCR, time to response, progression-free survival (PFS), overall survival (OS), and safety.
Patients with advanced or metastatic NSCLC harboring a KRAS G12C mutation who were refractory to or had intolerance of prior immunotherapy and platinum-based treatment were eligible for enrollment on the trial. Having no active brain or spinal metastases was another requirement for enrollment.
The median patient age was 62 years, 79.0% of patients were male, and 80.7% had an ECOG performance status of 1. Additionally, 59.7% of patients had previously smoked, 95.0% had an adenocarcinoma subtype, and 83.2% did not have brain metastases. Previous lines of therapy included 1 in 51.3%, 2 in 42.0%, and 3 in 6.7%. The most common treatment was platinum-based chemotherapy and PD-1/PD-L1 inhibitors in 94.1%.
A deep response was observed in 30.8% of patients with more than 50% tumor reduction. The median follow-up was 10.4 months, and 34.2% of patients were still on study treatment. The median time to response was 1.41 months.
Currently, the majority of patients with a PR have ongoing responses, and the median DOR has not been reached (95% CI, 7.2-not evaluable [NE]). Responses were ongoing in 73.6% of patients at 6 months and 56.6% at 12 months.
The median PFS was 8.2 months (95% CI, 5.5-13.1). At 12 months, the PFS rate was 40.0%. The median OS was 13.6 months (95% CI, 10.9-NE). The 12-month OS rate was 54.6%.
Grade 3 or higher treatment-related adverse effects (TRAEs) occurred in 38.7% of patients, and serious AEs occurred in 19.3%. Additionally, 97.5% of patients experienced at least 1 any-grade AE. No grade 5 AEs were observed. Overall, 5% of patients discontinued treatment due to TRAEs.
TRAEs leading to dose interruption were observed in 37.8% of patients. Additionally, 18.5% had a dose reduction following TRAEs.
The most common TRAEs of any grade included anemia (56.3%), blood bilirubin increase (48.7%), alanine aminotransferase increase (35.3%), and aspartate aminotransferase increase (35.3%). Additionally, there were minimal gastrointestinal-related toxicities that were low-grade, which included nausea (5.9%) and vomiting (7.6%). It was noted that 1 patient had grade 3 nausea.
Reference
Shi Y, Fang J, Xing L, et al. Efficacy and safety of glecirasib (JAB-21822) monotherapy in patients with advanced NSCLC harboring KRAS G12C mutation: top-line results from a pivotal phase 2 study. Presented at the 2024 American Society of Clinical Oncology Plenary Series. April 30, 2024.